Our Services
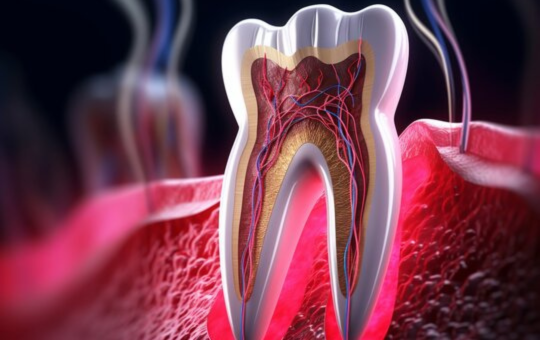
Root Canal
Diagnosis
Your dentist will first examine your tooth and take X-rays to determine the extent of the damage and whether a root canal is necessary.
Anesthesia
Before starting the procedure, the dentist will numb the area around the affected tooth using local anesthesia to ensure you don’t feel any pain during the procedure.
Access Opening
Once the area is numb, the dentist will create an opening in the crown of the tooth to access the pulp chamber and root canals.
Pulp Removal
Using small instruments, the dentist will remove the infected or damaged pulp tissue from the pulp chamber and root canals. They will also clean and shape the inside of the tooth to prepare it for filling.
Disinfection
After the pulp is removed, the dentist will thoroughly clean the inside of the tooth to remove any remaining bacteria or debris.
Filling
Once the tooth is cleaned and shaped, it will be filled with a biocompatible material called gutta-percha to seal the root canals and prevent further infection. The access opening in the crown will then be sealed with a temporary or permanent filling.
Restoration
In most cases, a tooth that has undergone a root canal will need a crown to protect it and restore its function and appearance. The crown is placed over the tooth after the root canal procedure is complete.
Follow-up
After the procedure, you may experience some discomfort or mild pain, which can usually be managed with over-the-counter pain medications. It’s essential to follow your dentist’s instructions for post-procedure care and attend any follow-up appointments to ensure proper healing.
Dental Implants

Initial Consultation
Your dentist will evaluate your oral health, take X-rays or CT scans, and discuss your medical history to determine if you’re a suitable candidate for dental implants.
Treatment Planning
Based on the evaluation, your dentist will develop a personalized treatment plan, including the number of implants needed, the placement location, and the type of restoration (crown, bridge, or denture).
Implant Placement
During the surgical procedure, the dentist or oral surgeon will make an incision in the gum tissue to expose the jawbone. They will then drill precise holes into the bone and place the implant screws. In some cases, immediate loading implants may be used, allowing for the attachment of temporary teeth on the same day.
Osseointegration
Over the next several months, the implants will integrate with the surrounding bone tissue through a process called osseointegration. This is crucial for the stability and success of the implants.
Abutment Placement
Once osseointegration is complete, small connectors called abutments are attached to the implants. These protrude above the gumline and serve as attachment points for the final restorations.
Final Restoration
Impressions of your teeth are taken to create custom-made dental crowns, bridges, or dentures. These restorations are then attached to the abutments, completing the implant-supported teeth.
Follow-up Care
After the procedure, regular follow-up appointments with your dentist are necessary to monitor healing and ensure the long-term success of the implants. Good oral hygiene practices and routine dental check-ups are also essential for maintaining the health of your implants and surrounding teeth.
Braces & Aligners

Initial Consultation
Your orthodontist will assess your teeth, jaws, and bite to determine if braces are the right treatment for you.
Treatment Planning
Based on the evaluation, your orthodontist will create a personalized treatment plan, including the type of braces (metal, ceramic, or lingual), duration of treatment, and specific adjustments needed.
Braces Placement
During this appointment, the orthodontist will:
- Clean and dry your teeth.
- Apply dental adhesive to attach brackets to the front surface of your teeth.
- Thread an archwire through the brackets and secure it in place using elastic bands or ligatures.
Follow-up Appointments
You’ll need to visit your orthodontist regularly for adjustments, usually every 4 to 6 weeks, where they will tighten or replace the archwire to continue guiding your teeth into alignment.
Monitoring Progress
Your orthodontist will closely monitor your progress to ensure that your teeth are moving correctly and that your bite is improving according to the treatment plan.
Retainer Phase
After your braces are removed, you’ll need to wear a retainer to maintain the new position of your teeth.
Initial Consultation
Your orthodontist will evaluate your teeth and discuss your treatment goals to determine if aligners are suitable for you.
Treatment Planning
Based on the evaluation, your orthodontist will create a digital treatment plan, including the number of aligners needed and the duration of treatment.
Impressions or Digital Scans
Impressions of your teeth are taken, or digital scans are performed to create a 3D model of your teeth, which is used to design your custom aligners.
Aligner Fabrication
Your aligners are fabricated based on the digital treatment plan, typically using advanced computer-aided design and manufacturing (CAD/CAM) technology.
Aligner Fitting
Once your aligners are ready, you’ll visit your orthodontist to ensure they fit properly and receive instructions on how to wear and care for them.
Follow-up Appointments
You’ll have periodic check-ups with your orthodontist to monitor your progress and receive new sets of aligners as needed.
Retainer Phase
After completing your aligner treatment, you may be advised to wear a retainer to maintain your results.
Child Dental Care

Early dental visits
Like in other countries, it’s recommended that children in India have their first dental visit by their first birthday or within six months of their first tooth eruption. However, in some cases, access to dental care may be limited, especially in rural areas, leading to delayed dental visits.
Preventive care
Preventive measures such as dental check-ups, cleanings, fluoride treatments, and dental sealants are important for maintaining good oral health in children. Community-based programs and school dental health programs may play a significant role in providing preventive care, particularly in underserved areas.
Education on oral hygiene
Dental professionals in India emphasize educating children and parents on proper oral hygiene practices, including brushing, flossing, and a balanced diet. This education may be delivered through dental clinics, schools, community health centers, and outreach programs.
Treatment of cavities
If a child develops a cavity, the dentist will remove the decayed portion of the tooth and fill the cavity with a dental filling material, such as composite resin or amalgam. In cases of extensive decay, a dental crown may be necessary to restore the tooth’s structure and function.
Orthodontic evaluation
Dentists assess the alignment of a child’s teeth and jaw to identify any orthodontic issues early on. Early intervention with orthodontic treatment, such as braces or orthodontic appliances, can help guide the growth of the jaws and teeth and prevent more serious orthodontic problems later in life.
Emergency dental care
Dentists are trained to handle dental emergencies in children, such as knocked-out teeth, broken teeth, or dental trauma. Prompt treatment is essential to save the tooth and prevent further complications.
Sedation dentistry
For children who are anxious or unable to tolerate dental procedures due to fear or special needs, sedation options ranging from nitrous oxide (laughing gas) to general anesthesia may be available to ensure a comfortable and stress-free experience.
Gum Treatments

Professional Dental Cleaning (Scaling and Root Planing)
This procedure involves the removal of plaque and tartar (hardened plaque) from the teeth and gumline. It helps to prevent and treat gum disease by eliminating bacteria and irritants that can lead to inflammation and infection.
Gum Grafting
Gum grafting is a surgical procedure used to cover exposed tooth roots or to augment thin gum tissue. It involves taking tissue from the roof of the mouth or another donor source and attaching it to the receded gums to improve their appearance and protect the tooth roots.
Pocket Reduction Surgery
In advanced cases of gum disease (periodontitis), pockets can form between the gums and teeth, allowing bacteria to accumulate and cause further damage. Pocket reduction surgery, also known as flap surgery, involves lifting the gums to remove tartar and bacteria from the root surfaces and then securing the gums back in place to reduce pocket depth.
Gingivectomy
This surgical procedure is used to remove excess gum tissue that may be overgrown or covering a portion of the teeth. Gingivectomy can improve the appearance of the gums and make it easier to clean the teeth effectively.
Laser Gum Therapy
Laser technology is increasingly being used in gum treatment to remove diseased gum tissue, disinfect periodontal pockets, and promote gum regeneration. Laser gum therapy is minimally invasive and can result in faster healing and reduced discomfort compared to traditional surgery.
Antibiotic Therapy
Antibiotics may be prescribed in conjunction with other gum treatments to control bacterial infection and inflammation. They can be administered orally, topically (as mouth rinses), or placed directly into periodontal pockets.
Maintenance Therapy
Following gum treatment, regular maintenance visits to the dentist or periodontist are crucial for monitoring gum health, performing professional cleanings, and providing ongoing care to prevent recurrence of gum disease.
Tooth Filling

Examination and Diagnosis
The dentist begins by examining the tooth and may take X-rays to determine the extent of the decay or damage. They will discuss treatment options with the patient and develop a plan based on the findings.
Anesthesia
Before the filling procedure begins, the dentist administers local anesthesia to numb the tooth and surrounding area. In some cases, especially for children or patients with dental anxiety, sedation options may be available to help them relax during the procedure.
Removal of Decay
Using a dental drill, laser, or air abrasion instrument, the dentist removes the decayed or damaged portion of the tooth. This leaves behind a clean, cavity-free area that is ready to be filled.
Preparation of the Tooth
The dentist prepares the tooth surface to receive the filling material. This may involve etching or applying a bonding agent to help the filling material adhere securely to the tooth structure.
Placement of Filling Material
The dentist places the chosen filling material into the prepared cavity or area of the tooth. There are several types of filling materials available, including:
- Composite Resin: Tooth-colored composite fillings are made of a mixture of plastic and glass materials. They can be customized to match the color of the natural tooth, making them aesthetically pleasing for visible teeth.
- Amalgam: Amalgam fillings, also known as silver fillings, are made of a combination of metals, including silver, mercury, tin, and copper. They are durable and suitable for filling cavities in the back teeth where chewing forces are greatest.
- Glass Ionomer: Glass ionomer fillings release fluoride and are often used for small cavities in areas with low chewing pressure, such as near the gumline or in baby teeth.
- Gold: Gold fillings are highly durable and long-lasting but less commonly used due to their higher cost and aesthetic considerations.
Shaping and Polishing
Once the filling material is placed, the dentist shapes and polishes it to ensure a smooth surface that matches the contour of the tooth. This helps restore the tooth’s function and aesthetics while preventing food accumulation and plaque buildup.
Post-Procedure Care
After the filling procedure, the patient may experience some sensitivity to hot and cold temperatures, but this usually subsides within a few days. Good oral hygiene practices, including regular brushing, flossing, and dental check-ups, are essential for maintaining the health of the filled tooth and preventing future cavities.
Crown & Bridges

Purpose
A dental crown, also known as a cap, is a prosthetic restoration that covers and encases a damaged or weakened tooth to restore its strength, shape, size, and appearance.
Materials
Crowns can be made from various materials, including porcelain, ceramic, metal alloys (such as gold or silver), or a combination of materials. Porcelain crowns are popular for their natural appearance and ability to blend seamlessly with surrounding teeth.
Procedure
- Examination and Preparation: The dentist begins by examining the tooth and may take X-rays to assess its condition. If a crown is deemed necessary, the tooth is prepared by removing a portion of its outer surface to make room for the crown.
- Impressions: After the tooth is prepared, impressions or digital scans are taken to create a custom-made crown that fits precisely over the tooth.
- Temporary Crown: While the permanent crown is being fabricated in a dental laboratory, a temporary crown may be placed over the prepared tooth to protect it.
- Placement: Once the permanent crown is ready, the temporary crown is removed, and the permanent crown is cemented or bonded onto the tooth using dental adhesive. The dentist checks the fit and bite to ensure proper alignment and function.
Uses
Dental crowns are used to restore teeth that are severely decayed, fractured, weakened, discolored, or misshapen. They can also cover dental implants or anchor dental bridges.
Purpose
A dental bridge is a fixed prosthetic device used to replace one or more missing teeth by spanning the gap between adjacent teeth or dental implants.
Types
There are several types of dental bridges, including traditional bridges, cantilever bridges, and Maryland (resin-bonded) bridges. Traditional bridges consist of one or more artificial teeth (pontics) anchored to adjacent natural teeth or dental implants using dental crowns.
Procedure
- Examination and Preparation: Similar to dental crowns, the dentist examines the teeth and prepares the abutment teeth (the adjacent teeth that will support the bridge) by removing a portion of their enamel.
- Impressions: Impressions or digital scans are taken to create a custom-made bridge that fits accurately over the prepared teeth.
- Temporary Bridge: While the permanent bridge is being fabricated, a temporary bridge may be placed to maintain the space and protect the exposed teeth.
- Placement: Once the permanent bridge is ready, the temporary bridge is removed, and the permanent bridge is cemented or bonded into place. The dentist ensures proper fit, alignment, and bite.
Uses
Dental bridges are used to restore function and aesthetics to the mouth by replacing missing teeth, improving chewing and speaking abilities, maintaining facial shape, and preventing remaining teeth from shifting out of position.
Laser Treatment

Gum Contouring
Dental lasers can be used to reshape and sculpt the gums to improve the appearance of a “gummy” smile or to create a more symmetrical gumline.
Gingivectomy
Laser gingivectomy involves the removal of excess gum tissue to treat conditions such as gum disease (gingivitis) or to expose more of the tooth surface for restorative or cosmetic purposes.
Frenectomy
This procedure involves the removal of a small fold of tissue (frenulum) that connects the lips, tongue, or cheeks to the gums or underlying tissue. Laser frenectomy can be used to treat conditions such as tongue-tie (ankyloglossia) or lip-tie.
Gum Disease Treatment
You’ll have periodic check-ups with your orthodontist to monitor your progress and receive new sets of aligners as needed.
Cavity Preparation
Dental lasers can be used to remove decayed tooth structure during cavity preparation. Laser technology allows for more precise and conservative removal of decay while preserving more healthy tooth structure compared to traditional drilling methods.
Tooth Desensitization
Laser therapy can help alleviate tooth sensitivity by sealing exposed dentin tubules and blocking pain transmission.
Dental Surgery
Lasers can be used for various oral surgical procedures, including removing small lesions or tumors, exposing impacted teeth, and performing biopsies.
Teeth Whitening
Laser-assisted teeth whitening procedures use dental lasers to activate whitening agents and accelerate the bleaching process, resulting in brighter and whiter teeth.
Gum Depigmentation
Laser gum depigmentation involves removing dark pigmentation or spots from the gums to improve their appearance and achieve a more uniform color.
Precision
Dental lasers allow for precise tissue targeting and removal, minimizing damage to surrounding tissues.
Minimally Invasive
Laser procedures often require less or no anesthesia and result in minimal bleeding, swelling, and discomfort.
Reduced Healing Time
Laser treatment promotes faster healing and tissue regeneration compared to traditional surgical techniques.
Sterilization
The heat generated by dental lasers has a sterilizing effect, reducing the risk of infection.
Tooth Extraction

Examination and Diagnosis
Before performing a tooth extraction, the dentist or oral surgeon will conduct a thorough examination of the affected tooth and surrounding tissues. This may involve taking X-rays to assess the tooth’s position, root structure, and relationship to nearby structures.
Anesthesia
To ensure the patient’s comfort during the procedure, local anesthesia is administered to numb the tooth and surrounding tissues. In some cases, especially for more complex extractions or for patients with dental anxiety, sedation options such as nitrous oxide (laughing gas) or intravenous (IV) sedation may be offered.
Extraction Procedure
- Loosening the Tooth: Using specialized dental instruments, the dentist or oral surgeon gently loosens the tooth from its socket in the jawbone. This may involve rocking the tooth back and forth to widen the socket and separate the tooth’s attachments.
- Extraction: Once the tooth is sufficiently loosened, it is carefully extracted from the socket using forceps or dental elevators. In some cases, particularly for impacted teeth (teeth that are partially or fully trapped beneath the gumline), a surgical extraction may be necessary. This involves making an incision in the gum tissue to access and remove the tooth.
- Bone Trimming: In certain cases, such as when a tooth is impacted or when bone irregularities are present, the dentist may need to trim or reshape the surrounding bone to facilitate tooth removal.
Post-Extraction Care
- Gauze Placement: After the tooth is removed, the dentist places a piece of sterile gauze over the extraction site to control bleeding and promote blood clot formation. The patient is instructed to gently bite down on the gauze to apply pressure to the extraction site.
- Pain Management: The dentist may prescribe pain medication or recommend over-the-counter pain relievers to manage post-extraction discomfort. Applying ice packs to the face can also help reduce swelling and discomfort.
- Activity Restrictions: Patients are typically advised to avoid strenuous activities, vigorous rinsing, and drinking through a straw for the first few days following the extraction to prevent dislodging the blood clot and promoting healing.
- Follow-Up: Patients are scheduled for a follow-up visit to monitor healing and remove any sutures (if necessary). The dentist will also provide instructions for proper oral hygiene and diet during the healing period.
Healing Process
The extraction site typically heals within a few weeks, during which new bone and gum tissue gradually fill in the empty socket. It’s important for patients to follow their dentist’s post-extraction instructions closely to minimize the risk of complications such as infection or dry socket (loss of the blood clot).
Tooth Cleaning

Preparation
Before the cleaning procedure begins, the dental hygienist or dentist may review the patient’s medical history and discuss any concerns or oral health issues. They may also perform a preliminary examination of the teeth and gums to identify areas of plaque or tartar buildup.
Scaling
The dental hygienist or dentist uses specialized dental instruments, such as scalers or ultrasonic scalers, to remove plaque and tartar from the tooth surfaces, including along the gumline and between the teeth. Scaling involves gently scraping away the hardened deposits without causing damage to the tooth enamel.
Root Planing (Deep Cleaning)
In cases of more advanced gum disease (periodontitis), root planing may be performed to remove plaque, tartar, and bacteria from below the gumline and to smooth the root surfaces of the teeth. This helps prevent further plaque buildup and promotes gum tissue healing.
Polishing
After scaling and root planing, the dental hygienist or dentist uses a polishing instrument and a gritty toothpaste-like substance to polish the teeth and remove surface stains. Polishing leaves the teeth smooth and shiny, making it more difficult for plaque to adhere to the tooth surfaces.
Fluoride Treatment (Optional)
Some dental offices offer fluoride treatment as part of the cleaning procedure. Fluoride is applied to the teeth in the form of a gel, foam, or varnish to strengthen the tooth enamel and protect against tooth decay. It may be particularly beneficial for patients at higher risk of cavities.
Final Examination
After the cleaning is completed, the dentist may perform a final examination of the teeth and gums to assess oral health and identify any areas of concern. They may also discuss oral hygiene practices and provide recommendations for maintaining good oral health between dental visits.
Post-Cleaning Instructions
The dental hygienist or dentist may provide instructions on proper oral hygiene techniques, including brushing, flossing, and using interdental cleaners or mouth rinses. They may also recommend dietary and lifestyle changes to support optimal oral health.
Disimpaction

Evaluation and Diagnosis
Before performing a disimpaction, the dentist or oral surgeon conducts a comprehensive evaluation, which may include dental X-rays or other imaging studies to assess the position, orientation, and relationship of the impacted tooth to surrounding structures.
Anesthesia
To ensure the patient’s comfort during the procedure, local anesthesia is typically administered to numb the affected area. In some cases, particularly for more complex or multiple extractions, sedation options such as nitrous oxide (laughing gas) or intravenous (IV) sedation may be offered to help the patient relax.
Exposure of the Impacted Tooth
Depending on the location and orientation of the impacted tooth, the dentist may need to make an incision in the gum tissue to access and expose the tooth. In some cases, a small amount of bone may need to be removed to fully expose the tooth.
Extraction of the Impacted Tooth
Once the impacted tooth is fully exposed, the dentist or oral surgeon uses specialized instruments to gently remove it from its position within the jawbone. The tooth may need to be sectioned (divided into smaller pieces) to facilitate removal, particularly if it is impacted deeply or positioned at an angle.
Closure and Healing
After the impacted tooth is extracted, the surgical site is thoroughly cleaned, and any incisions are closed with sutures (stitches). The dentist may place gauze over the extraction site to control bleeding and promote blood clot formation. The patient is provided with instructions for post-operative care, including pain management, oral hygiene, and dietary restrictions.
Follow-Up
Patients are typically scheduled for a follow-up visit to monitor healing and remove any sutures (if necessary). The dentist or oral surgeon may also perform additional imaging studies to assess bone healing and ensure that no complications have arisen.
Full Mouth Rehabilitation

Comprehensive Examination and Diagnosis
- The first step in full mouth rehabilitation is a comprehensive dental examination, including a review of the patient’s medical and dental history, clinical examination of the teeth, gums, jaw joints (TMJ), and occlusion (bite), as well as diagnostic imaging such as X-rays, CT scans, or digital impressions.
- The dentist or prosthodontist evaluates the condition of the teeth, gums, and supporting structures, identifies any existing dental problems or conditions (such as tooth decay, gum disease, tooth wear, misalignment, or missing teeth), and determines the underlying causes of these issues.
Treatment Planning
- Based on the findings of the examination and diagnosis, a personalized treatment plan is developed to address the patient’s specific dental needs, goals, and concerns.
- The treatment plan may involve a combination of restorative, prosthetic, periodontal, endodontic, orthodontic, and/or cosmetic dental procedures, depending on the complexity and extent of the dental problems.
Restorative and Prosthetic Procedures
- Restorative procedures may include dental fillings, root canal therapy, dental crowns, bridges, inlays, onlays, or dental implants to repair damaged or decayed teeth and restore their function and aesthetics.
- Prosthetic procedures may involve the fabrication and placement of partial or full dentures, implant-supported dentures, or fixed dental prostheses (such as bridges or implant-supported crowns) to replace missing teeth and restore chewing ability and facial aesthetics.
Periodontal Therapy
If gum disease (periodontitis) is present, periodontal therapy may be necessary to treat gum inflammation, infection, and bone loss. This may include deep cleaning (scaling and root planing), gum surgery (flap surgery), or periodontal maintenance to manage gum health.
Orthodontic Treatment
Orthodontic treatment, such as braces or clear aligners, may be recommended to correct misaligned teeth, malocclusion (poor bite), or jaw discrepancies and achieve proper tooth alignment and occlusion.
Cosmetic Dentistry
Cosmetic dental procedures, such as teeth whitening, dental veneers, dental bonding, or gum contouring, may be included to enhance the appearance of the smile and improve dental aesthetics.
Ongoing Maintenance and Follow-Up
- Following completion of the full mouth rehabilitation, regular dental check-ups, professional cleanings, and maintenance visits are essential to monitor oral health, prevent future dental problems, and ensure the longevity of the restorations.
- Patients are educated on proper oral hygiene practices and provided with customized oral care instructions to maintain their newly restored smile.